Celebrating Delta Center’s impact on the safety net
Kelsey Stefanik-Guizlo reflects on ACT Center’s 7-year partnership to improve care for communities in 19 states
By Kelsey Stefanik-Guizlo, MPH, a collaborative scientist with the Center for Accelerating Care Transformation (ACT Center) at Kaiser Permanente Washington Health Research Institute
Community health centers (CHCs) and community mental health centers (CMHCs) are the backbone of the U.S. health care safety net, serving about 38 million people nationwide. These organizations help ensure that communities that are not well served by traditional health care systems have access to essential physical and behavioral health services. The Delta Center for a Thriving Safety Net (Delta Center) was launched in 2018 with the support of the Robert Wood Johnson Foundation to help build collaborations that strengthen these vital services.
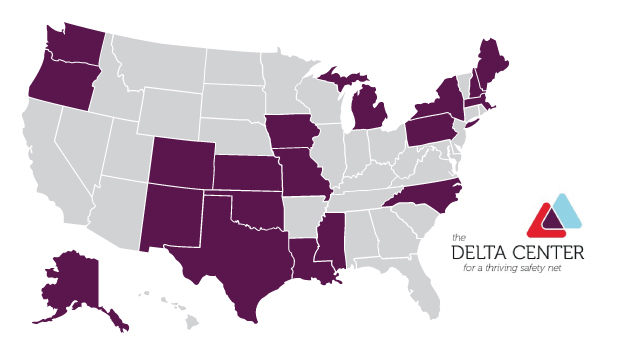
Over the past 7 years, the Delta Center has supported collective action projects in 19 states, engaging state primary care associations (PCAs) and behavioral health state associations (BHSAs) to advance policies and practices to better serve their communities. Led by JSI Research and Training Institute, Inc, the Delta Center offered monthly individual state-level coaching, developed written technical assistance briefs and materials, and hosted 6 multi-day in-person convenings and frequent webinars to facilitate cross-state learning. The ACT Center was proud to be among Delta Center’s partner organizations, which included the National Association for Community Health Centers and the National Council for Mental Wellbeing.
As the initiative concludes, we have an important opportunity to reflect on what contributed to the Delta Center’s success — and what key challenges remain for communities and providers in the safety net.
Why bring PCAs and BHSAs together to influence system change?
Initially, the aim of the Delta Center was to create a scalable, replicable model to build the capacity and strength of the safety net. We decided to work through PCAs and BHSAs because, as the state membership organizations that represent CHCs and CMHCs, they exist in every state. When they work together, they can have a powerful voice in shaping state policy and supporting their members to improve the care for marginalized communities. However, despite common goals and activities, PCAs and BHSAs often work in silos with limited coordination across their efforts.
That’s where the Delta Center saw an opportunity to help. Our primary goal was to foster collaboration and collective action between primary care and behavioral health organizations at the national, state, and local levels. Additionally, we wanted to enhance the ability of state associations to ensure that changes in incentives and care systems meet the goals and needs of individuals and families. Ultimately, we hoped to elevate insights for state and national decision-makers to influence systems change.
To achieve these objectives, the Delta Center provided support to 2 cohorts of grantees in 19 states. Participating PCAs and BHSAs received funding, coaching, training, and technical assistance to work together on multi-year projects focused on policy and practice change. Delta Center partners also organized in-person and virtual convenings to share insights from national experts and opportunities for grantees to work together to facilitate cross-state learning.
Focusing on value-based payment and care in Delta Center phase 1
The first phase of the Delta Center (2018 to 2021) focused on bolstering PCAs’ and BHSAs’ ability to help their members advance value-based payment and care. However, within states, many grantees had never worked with each other before, so the early focus was on understanding organizational histories and financing mechanisms, building relationships, and identifying shared priorities.
The activities for this first phase were based on JSI and ACT Center’s previous work identifying the actions and infrastructure necessary to implement value-based pay and care improvements (see our Model for Advancing High Performance 2.0).
As coaches, we learned a lot working with the teams from Colorado, North Carolina, and Oregon and collaborating with our Delta Center partners to plan and facilitate national convenings:
- Building relationships between PCAs and BHSAs takes time but yields substantial benefits. Before embarking on their Delta Center projects, several PCAs and BHSAs had experienced weak, non-existent, or competitive relationships with each other. The Delta Center gave them the opportunity to better understand one another, identify shared goals, and collaborate meaningfully.
- Buy-in from state Medicaid agencies and Medicaid managed care plans is critical. Having a clear vision for how to leverage data and apply value-based payment was essential to the associations’ efforts to ensure that high-value services were being delivered in communities served by the safety net.
Elevating equity and consumer voice in Delta Center phase 2
The second phase of the Delta Center (2021 to 2024) took place in a much different context. When the application period opened, PCAs and BHSAs were still grappling with COVID-19 and working through uncertainty related to telehealth practice and reimbursement, workforce shortages, and more. Additionally, the Delta Center brought forth a stronger focus on elevating consumer voices and advancing racial equity.
The ACT Center continued to play an important role, providing technical assistance to 2 states (New Hampshire and Oklahoma) and playing a key role in planning and facilitating in-person and virtual convenings. We also interviewed grantees in conservative states to learn about their efforts to advance health equity through policy. Our team is currently writing a paper to share insights from this process, as well as co-leading the final phase 2 evaluation report with JSI. We will be presenting findings from both projects at the AcademyHealth 2024 Conference on the Science of Dissemination and Implementation in December. Our key learnings include:
- Relationships beget relationships. We saw how strengthening the PCA/BHSA partnership enhanced collaborations with other key partners, such as state legislators and Medicaid agencies, public health departments, and Medicaid managed care plans.
- Consumer engagement can be feasible for PCAs and BHSAs. Many associations report challenges with consumer engagement since they don’t have direct access to consumers. But partnerships with state-level consumer advocacy associations can be an effective way to bring consumers into policy- and practice-change efforts.
- Progress on health equity policy is possible even in polarized state political contexts. PCAs and BHSAs are finding ways to advance health equity policy through intentional relationship building and tailoring their language choices to avoid politicized terms such as “diversity, equity, and inclusion” and instead focus on more politically palatable issues such as rural health or socioeconomic status.
2 key lessons we’re taking forward from the Delta Center
After 7 years of rewarding collaboration, the ACT Center is grateful for all that we learned working alongside our Delta Center partners — including these 2 overarching insights:
- Complex challenges require multifaceted solutions. The challenges facing the safety net are numerous: adequate access to high-quality care for patients, integration between physical health and behavioral health care, financial stability for CHCs and CMHCs, workforce shortages, and many more. By providing space for relationship building, access to expertise from regional and national experts, and opportunities for cross-state sharing, the Delta Center helped grantees make progress on these complex issues.
- Supporting PCAs, BHSAs, and other organizations that work within states to bolster the safety net is a promising and powerful way to make meaningful change. PCAs and BHSAs are excellent change agents for evidence-based policy change and practice improvement. They are deeply attuned to the needs of their members and savvy and adaptable in navigating state policy environments. Engaging these associations that are already knee-deep in the work to co-design project goals, activities, and outcomes leads to greater impact and helps ensure that initiatives like Delta Center are successful.
Support for this work was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the Robert Wood Johnson Foundation.




