Rapid engagement promotes person-centered access for Oregon behavioral health

A system in crisis cannot serve people in crisis and needs to transform
By Ariel Singer. Originally published by The Delta Center for a Thriving Safety Net.

Since 2018, the Center for Accelerating Care Transformation (ACT Center) has supported The Delta Center for a Thriving Safety Net (Delta Center) grantees in Oregon and several other states by providing technical assistance and hands-on coaching. Ariel works with the Delta Center to partner with consumers to transform behavioral health services in Oregon.
Ariel worked at the Oregon Primary Care Association (OPCA) during the initial round of Delta Center funding and led OPCA’s partnership with the Association of Oregon Community Mental Health Programs (AOCMHP) as part of a Delta Center grant from 2018-2021. Since leaving OPCA in 2021, she has worked with AOCMHP to lead multi-stakeholder planning and pilot implementation of Rapid Engagement, a behavioral health access innovation. Funding from the Delta Center and the Oregon Health Authority made it possible for AOCMHP to convene a diverse group of stakeholders to address policy, payment, and clinical practice change strategies for designing and launching the Rapid Engagement pilot.
Nationwide, we have seen a tremendous increase in demand for behavioral health services in the last several years. In Oregon, the behavioral health system was already struggling from historic underinvestment and lack of payment parity with physical health settings. Rapid Engagement is a behavioral health access innovation in Oregon that’s trying to make it easier, faster, and more user-friendly for people in need to get started with services. Rapid Engagement is a trauma-informed and person-centered approach and was inspired by the Treat First model in New Mexico. The population of the state has grown, and the behavioral health care system has not been able to keep pace by adding capacity. There is widespread recognition in the state that Oregon’s system for supporting people with behavioral health challenges is stressed.
Even before this latest era of difficulties, there have been far too many obstacles for people to get prompt and low-barrier access to behavioral health treatment. With the Rapid Engagement approach, providers have more flexibility in their early interactions to spend their time building trust, establishing therapeutic relationships, and meeting client needs. This flexibility allows them to focus on understanding and responding to consumer priorities rather than system requirements. With funding from the Oregon Health Authority, the Rapid Engagement pilot started last fall and 5 provider organizations from urban, rural, and frontier corners of Oregon are testing and improving this new approach to bringing people into services.
Sharing a personal story is a powerful way to bring attention to the importance of system change. In this blog post, I’ll take you through my own recent experience getting started with behavioral health services, and how this experience shaped my views on why giving people an easier, faster, and more user-friendly way to access services is so important. More importantly, I’ll also showcase an Oregon Health Plan consumer’s Rapid Engagement experience, which underscores the important connection of this work to improving health equity.
Imagine a System Designed for Consumers Instead of Requirements
For most of my career in health system transformation, I have worked on quality improvement in primary care. In primary care settings, our operating model expects that people will need treatment over time, for both preventive and acute needs, and that when someone comes in for care, a brief history and treatment plan can be drawn up in a 20-minute visit.
This past fall, I was going through a lot of changes in my personal life, and I wanted to engage with counseling for therapeutic support during this time of significant transition. To get help from a counselor, I started by contacting my health care provider’s behavioral health department to request an appointment. “No problem,” they said. “We have an appointment available in just a few weeks.” Having been concerned about long wait times, I was thrilled to learn that I would only have to wait a couple of weeks to speak to a therapist.
When I logged on for the virtual visit, the therapist was kind and warm and asked me a lot of questions about my life. This was no primary care visit; she spent nearly an hour asking me wide-ranging questions about my life. At the end of this conversation, she said, “I really wish I could work with you, but I just do the intakes and you will have to call this other number to get started with a therapist who will provide treatment.” Sigh.
When I finally got connected to the treating clinician, she proceeded to ask me all the same questions that the intake clinician had asked. She had not received any of these details from the initial conversation, and I had to spend a second hour of my time answering questions instead of receiving support. It was not until the third hour of interacting with the system that space was made for my priorities – the first two hours were dedicated entirely to meeting system requirements.
This set of experiences was a deterrent even for me, a highly educated and motivated patient. Even though I was willing and able to go through two hours of assessment before being offered any therapeutic support, it amplified my desire to reduce the barriers to getting care. While this experience got an eyeroll from me, its impact on some individuals can be much more significant. Lengthy intake and assessment processes can hinder engagement for individuals with ambivalence towards seeking behavioral health services, as well as those who are facing time-consuming social or financial challenges, or dealing with complex mental, substance use, or physical health issues. If we don’t change how we do things, we risk alienating those who might need help the most.
A System in Crisis Cannot Serve People in Crisis
From the beginning of designing Rapid Engagement, we have tried to put the people we serve at the center. We conducted consumer focus groups and interviews and collaborated with members of the peer workforce to develop the Rapid Engagement model. A consumer named Carl agreed to sit down with me one rainy, grey day last spring. He told me his story of lifelong behavioral health challenges, the impact on his health and well-being, and his struggle to get help. Despite the difficulties he faced, getting into treatment and supportive housing has made a huge difference in his life.
Like me, Carl described being asked an extensive series of questions when he tried to enroll in care. Unfortunately for Carl, he has less resilience than I did to deal with this assessment process. He describes how painful it felt for him to answer all those questions, “When you’re meeting somebody, you don’t want to tell ‘em about all your abuses. It’s embarrassing to talk about some of that stuff that has happened to me and stuff that I have perpetrated on other people.”
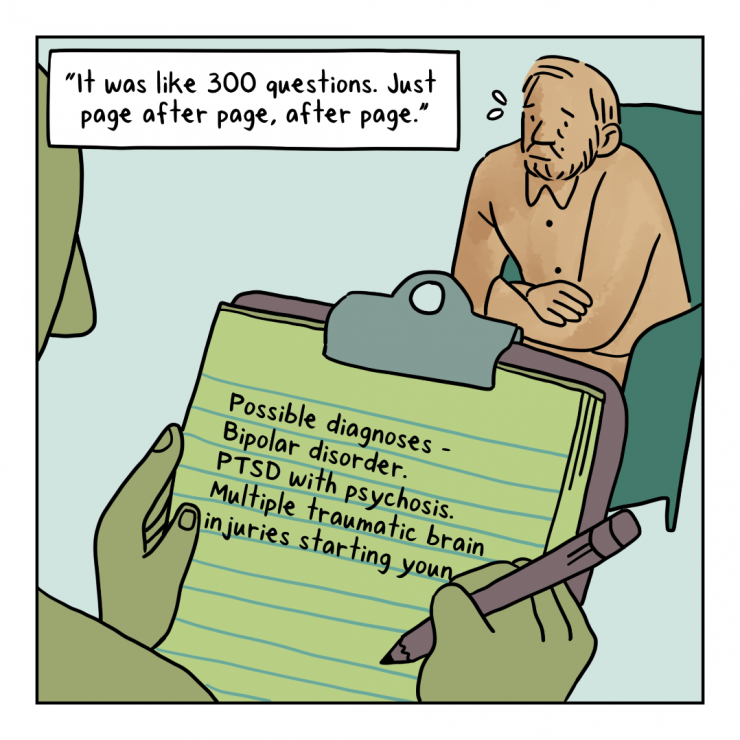
Also like me, Carl thinks there must be a faster and easier way to get people started with therapy, “I talked to this fellow and I thought he and I were going to do something together…it was like 300 questions. Just page after page, after page. I think potentially it could be streamlined to get to the right people in a timely fashion. You know, 10 or 15 questions about what that individual needs.”
Transformation is Underway
There are still a variety of operational challenges to sort out. But the participating organizations report enthusiasm from their staff for this approach, sustained conviction that Rapid Engagement allows them to provide better service to their clients, and a sense that Rapid Engagement is particularly helpful for people like Carl, who are already experiencing a lot of barriers to access.
Even though we are starting out with Rapid Engagement as a pilot for members of Oregon’s Medicaid program, I hope to see Rapid Engagement succeed as a pilot and become the status quo approach for outpatient behavioral health intakes statewide Across payers and settings, it shouldn’t take 2 hours of assessment to get people started. It shouldn’t be the norm that all of the system requirements are met before any of the consumer’s priorities are met.
We still have a lot to learn about how best to implement and scale Rapid Engagement, and we already know that Rapid Engagement alone will not solve Oregon’s or the nation’s behavioral health access challenges. We also know that when people engage in services, behavioral health treatment works. So, let’s make behavioral health access faster, easier, and more user-friendly for everyone, especially those who need it the most.



