Research helps our newest clinics build the future — now

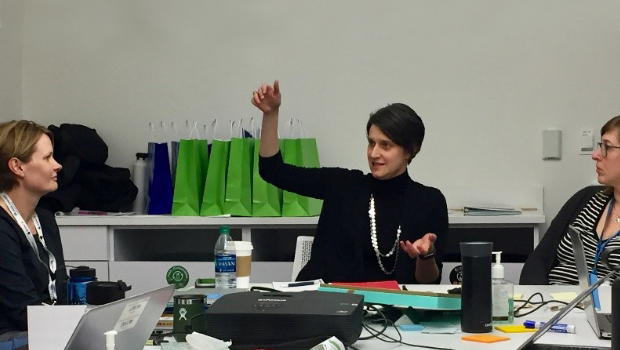
L-R: Hannah Burdge, DO, South Lake Union Medical Office Building Chief; Esther Hong, South Lake Union Medical Office Building manager; Paula Lozano, MD, MPH, Kaiser Permanente Washington’s senior associate medical director for research and translation; Katie Coleman, MSPH, director of KPWHRI’s MacColl Center for Health Care Innovation and KPWA Learning Health System Program, and Jennifer Meyer, MD, Ballard Medical Center pediatrician.
Katie Coleman tells how Kaiser Permanente Washington research supports innovation at new clinics in Ballard and South Lake Union
Katie Coleman, MSPH, answered our questions about the involvement of Kaiser Permanente Washington’s Learning Health System Program in designing and evaluating an innovative staffing model at the newest clinics in Seattle’s South Lake Union and Ballard neighborhoods. Ms. Coleman is director of Kaiser Permanente Washington Health Research Institute (KPWHRI)’s MacColl Center for Health Care Innovation and the Learning Health System Program. She co-leads this effort with Maggie Jones, MPH, director of KPWHRI’s Center for Community Health and Evaluation (CCHE).
What excites you most about this work?
I am delighted that Kaiser Permanente Washington’s Innovation team is involving the Learning Health System Program in developing and evaluating these two newest primary care clinics, from the ground up. This is my favorite of all my projects. This is such a fun opportunity for us to help design an evidence-based model for the future of primary care—and give real-time feedback to evaluate it as we go. In partnership with our clinical colleagues, we’re developing new ways for teams to work together and provide care for patients in the way they want it, with access to the providers of their choice in person or virtually. And we’re seeing how well teams deliver on the promise of expanding use of technology, enhancing the well-being of staff and providers, and giving patients a convenient, accessible, and high-quality experience.
How did research inform clinic design?
In addition to Kaiser Permanente’s best practices, the MacColl Center’s prior research helped inform the staffing models for the clinics. I think the South Lake Union clinic is the first Kaiser Permanente facility to strongly follow MacColl’s recommendations for reorganizing teams to improve primary care. Made with the Agency for Healthcare Research and Quality, these recommendations specify full-time equivalent (FTE) levels for various team members including physicians, physician assistants, nurse practitioners, registered nurses (more than usual), social workers, therapists, pharmacists, care coordinators, population managers, quality improvement leaders, front desk staff, and medical assistants (MAs). We based these recommendations in part on a MacColl study called Learning from Effective Ambulatory Practices (LEAP), in which we saw that practices around the country functioned best when all team members practiced at the top of their license.
What makes the new clinics special?
They’re different in 4 ways: expanded teams, open access, virtual care at the clinic to promote continuity, and built-in time and support for local quality improvement. Our earlier research showed that primary care teams work well when their members are empowered to help solve patients’ problems. That’s part of the reason the new clinics are implementing a new enhanced role called a guide, who can do health coaching and help patients navigate the system. The goal is to employ 3 guides per clinician. And as at other Kaiser Permanente Washington clinics, South Lake Union and Ballard patients also have access to community resource specialists. A physical therapist is there—and a financial counselor from the new Bridging Care and Coverage program, to help patients, if necessary, at the end of their visit. These are also the first Kaiser Permanente Washington clinics to have a chiropractor on staff. And although the South Lake Union clinic doesn’t have room for an onsite pharmacy, it does have an InstyMeds dispenser that provides prescription medications.
L-R: Elizabeth Fleming, MBA, Kaiser Permanente Washington vice president for innovation and business development; Maggie Jones, MPH, director of KPWHRI’s Center for Community Health and Evaluation; and Katie Coleman, MSPH, director of KPWHRI’s MacColl Center for Health Care Innovation and Kaiser Permanente Washington’s Learning Health System Program.
What about access to care and managing populations?
The new clinics’ schedules build in dedicated time for team members to discuss workflow issues and brainstorm solutions—and see patients that same day, increasing access to care. Longer visit cycles allow time for collaboration and proactive care: Instead of pushing this work out to another day, the idea is that team members can connect patients with solutions and other relevant clinicians today. Access to care also happens through virtual care, with the clinic’s own providers answering patients’ questions on secure messaging and Care Chat.
How did the design process work?
Early on, the Innovation team engaged a variety of stakeholder groups with diverse perspectives, including patients, staff, and us researchers and evaluators. Through ethnographic analysis of people living in the neighborhood, they explored their health care needs and expectations. Later, Innovation set up a mockup layout of each clinic so that team members could conduct “simulations” of patient visits and staff workflows before the clinics opened.
As researchers and evaluators, part of our work has been to document this unique design process. We’re also collecting data to help with continuous improvement—and with learning lessons to help design the other clinics that Kaiser Permanente Washington plans to open soon. Working together, we’ll be able to determine which elements of the model really make a difference. Long term, we will assess this care model’s impact on patient and staff experience, health care utilization, care quality, health outcomes, cost of care, staff retention, and enrollment.
What have you learned so far?
We can share preliminary findings from South Lake Union:
- Compared to other Kaiser Permanente Washington clinics, it’s attracting a higher proportion of new members, many of whom work for Amazon, which is headquartered in the neighborhood.
- Clinic visits are about one third in person, one third by phone, and one third through secure messaging. That’s more online and fewer in-person visits than at the organization’s other clinics.
- South Lake Union patients and staff are reporting positive experiences there—more so than at other clinics.
Now the Ballard clinic is benefiting from these lessons. We helped design a template for the future of primary care. And that future is here.
Who is on the team?
We have a fantastic team at KPWHRI working on this project: In addition to Maggie Jones and me as leaders, Carly Levitz, MPH, a CCHE evaluation & learning associate, is participating in weekly team meetings at the new clinics to learn about the implementation of the model of care—and gather insights for continuous process improvement. Our team also includes Erin Hertel, MPA, Tyler Ross, MA, Sharon Fuller, Roy Pardee, JD, Melissa Anderson, MS, and Paula Blasi, MPH. We’ve also benefited from the support of the Learning Health System Program leadership team: Emily Westbrook, MHA, and Paula Lozano, MD, MPH.
Together, we nominated our Kaiser Permanente Washington colleagues at South Lake Union for the 2019 Birnbaum Award: South Lake Union Medical Office leaders Hannah Burdge, DO, Esther Hong, and Justin Hendricks; and Kaiser Permanente Washington Innovation team members Elizabeth Fleming, MBA, Connor Shea, MHA, Trina Davis, MD, Julie Song, and Ana Skwierinski, MS. Our Ballard team members include Jennifer Meyer, MD—and really the whole staff of 45.