How small health centers can improve care and thrive under value-based payment
The challenge
Primary care plays a crucial role as the backbone of a high-functioning health system, and community health centers (CHCs) provide much-needed primary care to millions of people across the country. CHCs are also laboratories for creative problem solving on issues ranging from how to utilize staff in expanded roles, to implementing unique strategies for addressing social needs, to leveraging local context to solve community-specific health problems.
As CHCs identify strategies to improve care, they are simultaneously seeking ways to ensure those improvements can be sustained by participating in value-based payment models. Caring for complex patients while remaining financially solvent requires infrastructure that is difficult to put in place for all health centers. But small health centers, defined as centers caring for fewer than 10,000 patients or having an operating budget of $10 million or less, face unique challenges in securing access to capital, building strong data capabilities, and negotiating favorable rates with vendors and health plans. Small CHCs need a roadmap for navigating care transformation and value-based care payment.
The work
Building on decades of experience working with CHCs and their partners through a variety of initiatives, including the Safety Net Medical Home Initiative and Learning from Effective Ambulatory Practices (LEAP), the MacColl Center for Health Care Innovation (now the ACT Center) partnered with John Snow, Inc. to produce the Model for Advancing High Performance (MAHP) to help small health centers deliver great care sustainably. 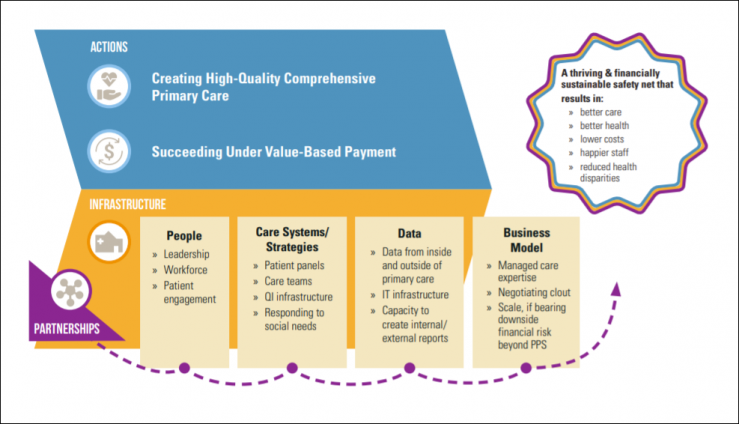
Based on research and expert opinion, the model clearly outlines the activities and infrastructure components small health centers need to achieve the quintuple aim — better care, better health, lower costs, happier staff, and reduced health disparities. The project also identifies 7 types of partnerships health centers can develop to support and supplement their primary care activities to improve health and leverage resources.
What we learned
The MAHP shows that engaging in the actions required to achieve the quintuple aim requires supportive infrastructure in four major areas: people, care systems/strategies, data, and a business model. Infrastructure elements like meaningful patient engagement in care, well-defined patient panels, and the ability to create actionable data reports are important to support both care transformation and value-based payment.
The 7 partnerships important for small health centers to explore in order to succeed with value-based payment and care include:
- Partnerships with community-based agencies and organizations (local government and nonprofit)
- Partnerships with hospitals
- Consortia
- Management services organizations and clinically integrated networks
- Health center-led independent practice associations (IPAs)
- Partnerships with health plans
- Mergers and acquisitions
Each of these partnership types has pros and cons, outlined in detail in our white paper: Partnering to Succeed: How Small Health Centers Can Improve Care and Thrive Under Value-Based Payment. The paper also includes 4 case studies that show how some health centers are creatively leveraging partnerships.
Impact
The MAHP model is the foundation for the Delta Center for a Thriving Safety Net’s Model for Advancing High Performance 2.0 (MAHP 2.0), a unified set of evidence-based actions and infrastructure necessary for CHCs and community behavioral health organizations to both provide high-quality, comprehensive primary care and succeed in value-based payment arrangements.
PROJECT SNAPSHOT
FUNDER
California Health Care Foundation
PARTNERS
JSI Research and Training Institute
KEY CONTRIBUTIONS
Model development
Evidence synthesis